Pes Planus What You Should Expect
Overview
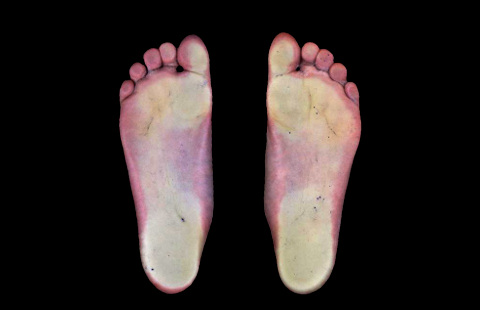
Flat feet, fallen arches, or ?pes planus? is normally a symptomless and fortunately painless condition. It is characterized by the arch of the foot collapsing completely, which causes the entire sole of the foot to come into perfect contact with the ground. An estimated 20-30 percent of the entire population has some form of flat feet, ranging in severity from asymptomatic to somewhat problematic. Most people who endure this problem are able to experience life pain and symptom free from the nearly unnoticeable abnormality. However, a small sector of those affected do experience pain or discomfort, which is when a treatment program needs to be put in action.
Causes
You can have a tendency towards fallen arches from birth. Up through the toddler stage, it is common to have flat feet. Throughout childhood, arches tend to normally develop. For reasons not well understood, however, in some cases the feet stay flat and the arch never forms. In many cases this abnormality does not cause symptoms or require any treatment. In other cases, it is due to a condition called tarsal coalition. This occurs when some of the foot bones fuse.
Symptoms
Arches can be seen as ?rolling downward? or collapsing when walking. Pain may present in lower back, hips or knees. Pain may be present on the bottom of the heels, within the arch, within the ankles or even the forefoot. Swelling can occur. Pain may occur in the anterior leg muscles.
Diagnosis
People who have flat feet without signs or symptoms that bother them do not generally have to see a doctor or podiatrist about them. However, if any of the following occur, you should see your GP or a podiatrist. The fallen arches (flat feet) have developed recently. You experience pain in your feet, ankles or lower limbs. Your unpleasant symptoms do not improve with supportive, well-fitted shoes. Either or both feet are becoming flatter. Your feet feel rigid (stiff). Your feet feel heavy and unwieldy. Most qualified health care professionals can diagnose flat feet just by watching the patient stand, walk and examining his/her feet. A doctor will also look at the patient's medical history. The feet will be observed from the front and back. The patient may be asked to stand on tip-toe while the doctor examines the shape and functioning of each foot. In some cases the physician may order an X-ray, CT (computed tomography) scan, or MRI (magnetic resonance imaging) scan.
arch support for flat feet
Non Surgical Treatment
If your condition is bothersome, try elevating your feet and using ice on the arches to reduce swelling. Your podiatrist can recommend several orthotic aids and inserts to strengthen the tendons of your foot. He can also demonstrate stretching exercises or refer you to physical therapy to get those tendons back into shape. If the symptoms of fallen arches are painful and troubling, he may recommend a steroid injection to relieve inflammation and pain. And in some instances, he may determine that surgery is necessary.
Surgical Treatment
Surgical correction is dependent on the severity of symptoms and the stage of deformity. The goals of surgery are to create a more functional and stable foot. There are multiple procedures available to the surgeon and it may take several to correct a flatfoot deformity. Stage one deformities usually respond to conservative or non-surgical therapy such as anti-inflammatory medication, casting, functional orthotics or a foot ankle orthosis called a Richie Brace. If these modalities are unsuccessful surgery is warranted. Usually surgical treatment begins with removal of inflammatory tissue and repair of the posterior tibial tendon. A tendon transfer is performed if the posterior tibial muscle is weak or the tendon is badly damaged. The most commonly used tendon is the flexor digitorum longus tendon. This tendon flexes or moves the lesser toes downward. The flexor digitorum longus tendon is utilized due to its close proximity to the posterior tibial tendon and because there are minimal side effects with its loss. The remainder of the tendon is sutured to the flexor hallucis longus tendon that flexes the big toe so that little function is loss. Stage two deformities are less responsive to conservative therapies that can be effective in mild deformities. Bone procedures are necessary at this stage in order to recreate the arch and stabilize the foot. These procedures include isolated fusion procedures, bone grafts, and/or the repositioning of bones through cuts called osteotomies. The realigned bones are generally held in place with screws, pins, plates, or staples while the bone heals. A tendon transfer may or may not be utilized depending on the condition of the posterior tibial tendon. Stage three deformities are better treated with surgical correction, in healthy patients. Patients that are unable to tolerate surgery or the prolonged healing period are better served with either arch supports known as orthotics or bracing such as the Richie Brace. Surgical correction at this stage usually requires fusion procedures such as a triple or double arthrodesis. This involves fusing the two or three major bones in the back of the foot together with screws or pins. The most common joints fused together are the subtalar joint, talonavicular joint, and the calcaneocuboid joint. By fusing the bones together the surgeon is able to correct structural deformity and alleviate arthritic pain. Tendon transfer procedures are usually not beneficial at this stage. Stage four deformities are treated similarly but with the addition of fusing the ankle joint.